Chapter 11: Cardiovascular Collapse and Sudden Death
Unexpected cardiovascular collapse and death most often result from ventricular fibrillation in pts with atherosclerotic coronary artery disease or underlying structural heart conditions. The most common etiologies are listed in Table 11-1. Arrhythmic causes may be provoked by electrolyte disorders (especially hypokalemia), hypoxemia, acidosis, or massive sympathetic discharge, as may occur in CNS injury. Immediate institution of cardiopulmonary resuscitation (CPR) followed by advanced life support measures (see below) is mandatory. Without institution of CPR within 4–6 min, ventricular fibrillation or asystole is usually fatal.
| Structural Associations and Causes |
|
| Functional Contributing Factors |
|
| Causes of Pulseless Electrical Activity Leading to Sudden Death |
|
MANAGEMENT OF CARDIAC ARREST
Basic life support (BLS) must commence immediately (Fig. 11-1):
FIGURE 11-1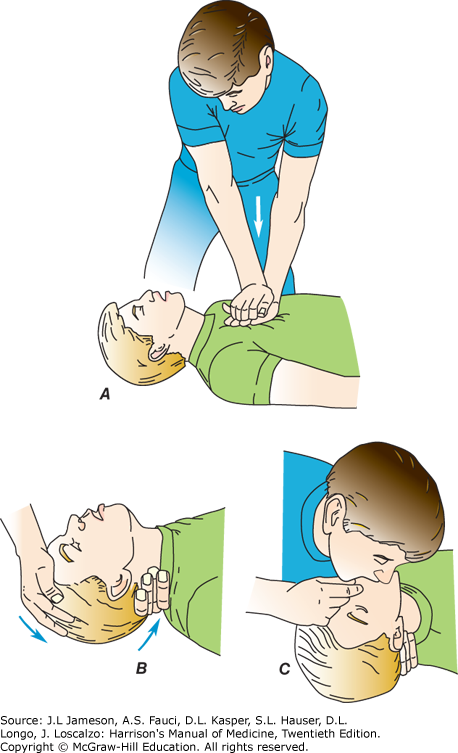
Major steps in cardiopulmonary resuscitation. A. Begin cardiac compressions at 100−120 compressions/min. B. Confirm that victim has an open airway. C. Trained rescuers begin ventilation if advanced life support equipment is not available (pocket mask preferred if available). (Modified from J Henderson: Emergency Medical Guide, 4th ed. New York, McGraw-Hill, 1978.)
- Phone emergency line (e.g., 911 in the United States); retrieve automated external defibrillator (AED) if available.
- If respiratory stridor is present, assess for aspiration of a foreign body and perform Heimlich maneuver.
- Perform chest compressions (depressing sternum 5 cm) at rate of 100−120 per min without interruption. A second rescuer should attach and utilize AED.
- If second rescuer is present and trained, tilt pt’s head backward, lift chin, and begin rescue breathing (pocket mask is preferable to mouth-to-mouth respiration to prevent transmission of infection), while chest compressions continue. The lungs should be inflated twice in rapid succession for every 30 chest compressions. For untrained lay rescuers, chest compression only, without ventilation, is recommended until advanced life support capability arrives.
- As soon as resuscitation equipment is available, begin advanced life support with continued chest compressions and ventilation. Although performed as simultaneously as possible, defibrillation (150–200 J biphasic) takes highest priority (Fig. 11-2), followed by establishment of IV access and insertion of an advanced airway (endotracheal tube or supraglottic) or bag-valve-mask device if an advanced airway cannot be achieved. One hundred percent O2 should be administered initially. Once an advanced airway is placed, ventilate at rate of 1 breath every 6–8 s without interrupting chest compressions.
- Initial IV access should be through the antecubital vein, but if drug administration is ineffective, an intraosseous or central line (internal jugular or subclavian) should be placed. IV NaHCO3 should be administered only if there is persistent severe acidosis (pH <7.15) despite adequate ventilation. Calcium is not routinely administered but should be given to pts with known hypocalcemia, to those who have received toxic doses of calcium channel antagonists, or if hyperkalemia is thought to be the triggering event for resistant ventricular fibrillation.
- The approach to cardiovascular collapse caused by asystole, other bradyarrhythmias, or pulseless electrical activity is shown in Fig. 11-3.
- Therapeutic hypothermia (cooling to 32–36°C [89.6–96.8°F] for at least 24 h) should be considered for unconscious survivors of cardiac arrest.
FIGURE 11-2
Management of cardiac arrest due to VF or VT. If metabolic acidosis persists after successful defibrillation and with adequate ventilation, also consider administration of 1 meq/kg NaHCO3. CPR, cardiopulmonary resuscitation; PCI, percutaneous coronary intervention; ROSC, return of spontaneous circulation; VF, ventricular fibrillation; VT, ventricular tachycardia. (Modified from HPIM-20, Figure 299-3A.)
FIGURE 11-3
Algorithms for bradyarrhythmia/asystole (left) or pulseless electrical activity (right) are dominated by cardiopulmonary resuscitation (CPR) and a search for reversible causes. MI, myocardial infarction. (From Albert CM, Stevenson WG: Cardiovascular collapse, cardiac arrest, and sudden cardiac death, in Jameson JL et al (eds). Harrison’s Principles of Internal Medicine, 20th ed. New York, NY: McGraw-Hill; 2018.)
FOLLOW-UP
If cardiac arrest resulted from ventricular fibrillation in initial hours of an acute MI, follow-up is standard post-MI care (Chap. 121: ST-Segment Elevation Myocardial Infarction). For other survivors of a ventricular fibrillation arrest, further assessment, including evaluation of coronary anatomy and left ventricular function is appropriate. In absence of a transient or reversible cause, placement of an implantable cardioverter defibrillator is usually indicated.
Citation
Kasper, Dennis L., et al., editors. "Chapter 11: Cardiovascular Collapse and Sudden Death." Harrison's Manual of Medicine, 20th ed., McGraw Hill Inc., 2020. harrisons.unboundmedicine.com/harrisons/view/Harrisons-Manual-of-Medicine/623013/all/Chapter_11:_Cardiovascular_Collapse_and_Sudden_Death.
Chapter 11: Cardiovascular Collapse and Sudden Death. In: Kasper DLD, Fauci ASA, Hauser SLS, et al, eds. Harrison's Manual of Medicine. McGraw Hill Inc.; 2020. https://harrisons.unboundmedicine.com/harrisons/view/Harrisons-Manual-of-Medicine/623013/all/Chapter_11:_Cardiovascular_Collapse_and_Sudden_Death. Accessed April 30, 2025.
Chapter 11: Cardiovascular Collapse and Sudden Death. (2020). In Kasper, D. L., Fauci, A. S., Hauser, S. L., Longo, D. L., Jameson, J. L., & Loscalzo, J. (Eds.), Harrison's Manual of Medicine (20th ed.). McGraw Hill Inc.. https://harrisons.unboundmedicine.com/harrisons/view/Harrisons-Manual-of-Medicine/623013/all/Chapter_11:_Cardiovascular_Collapse_and_Sudden_Death
Chapter 11: Cardiovascular Collapse and Sudden Death [Internet]. In: Kasper DLD, Fauci ASA, Hauser SLS, Longo DLD, Jameson JLJ, Loscalzo JJ, editors. Harrison's Manual of Medicine. McGraw Hill Inc.; 2020. [cited 2025 April 30]. Available from: https://harrisons.unboundmedicine.com/harrisons/view/Harrisons-Manual-of-Medicine/623013/all/Chapter_11:_Cardiovascular_Collapse_and_Sudden_Death.
* Article titles in AMA citation format should be in sentence-case
TY - ELEC
T1 - Chapter 11: Cardiovascular Collapse and Sudden Death
ID - 623013
ED - Jameson,J Larry,
ED - Loscalzo,Joseph,
ED - Kasper,Dennis L,
ED - Fauci,Anthony S,
ED - Hauser,Stephen L,
ED - Longo,Dan L,
BT - Harrison's Manual of Medicine
UR - https://harrisons.unboundmedicine.com/harrisons/view/Harrisons-Manual-of-Medicine/623013/all/Chapter_11:_Cardiovascular_Collapse_and_Sudden_Death
PB - McGraw Hill Inc.
ET - 20
DB - Harrison's Manual of Medicine
DP - Unbound Medicine
ER -

 Harrison's Manual of Medicine
Harrison's Manual of Medicine

